Insurance Eligibility & AR Services
Accurate Verification. Faster Payments. Reduced Denials.
CandyPharma provides reliable insurance eligibility verification and accounts receivable (AR) services to help healthcare providers minimize claim rejections, accelerate payments, and maintain a healthy revenue cycle.
Eligibility & AR Management Services
Accurate eligibility verification and proactive AR management to reduce denials, improve cash flow, and ensure timely reimbursements.
Our Services Include
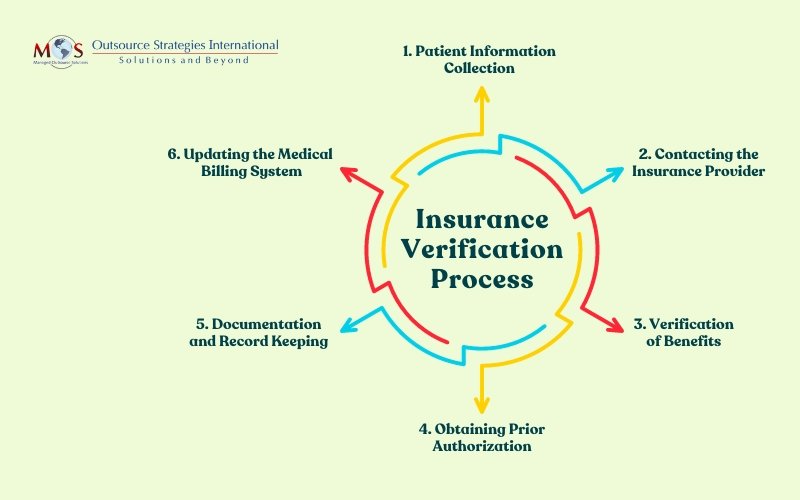
- Insurance eligibility & benefit verification
- Prior authorization support
- Claims follow-ups & AR management
- Denial analysis & resolution
- Payment posting & reconciliation
Why CandyPharma Eligibility & AR
- Reduced claim denials and delays
- Faster reimbursement turnaround
- Experienced AR & billing specialists
- HIPAA-compliant processes
- Transparent reporting & updates
Helping healthcare providers achieve accurate billing, faster collections, and stronger financial control.
